This week’s Image comes from Drs Wetendorf, Daul and Pennycuff, who treated a 43-year-old female patient in the ED who presented with acute onset of shortness of breath and chest pain. She was noted to be tachypneic and tachycardic. The patient had a history of recent bilateral quadriceps tendon repairs. 12-lead EKG showed evidence of right heart strain (S1Q3T3 pattern). A bedside echo was performed by ED physicians and the following was noted: RV dilatation, septal D-sign and bowing of inter-ventricular septum. The patient was immediately started on unfractionated heparin and sent over for CT PE study which showed extensive bilateral pulmonary emboli extending from both main pulmonary arteries into distal segments. A DVT study done several days later showed bilateral DVTs. In this case, the patient did not receive thrombolytics in the ED or during admission – in part due to recent surgery and the fact she remained hemodynamically stable in the ED and during her admission.
Bedside echo can be a very useful tool with pulmonary embolism for three reasons:
- As a screening test for the stable patient with undifferentiated chest pain or shortness of breath: visualizing echocardiographic signs of RV strain should raise the suspicion of PE in your differential diagnosis, and prompt the provider to consider ordering appropriate studies to rule in the diagnosis. It can facilitate earlier initiation of treatment with IV heparin prior to completion of radiology studies.
- In the unstable patient who is hypotensive or shows signs of shock with an appropriate clinical presentation, it can provide cognitive support to consider IV thrombolytics in the ED (especially if bedside compression studies are done as well and show clot in the legs). These patients are typically very challenging to manage traditionally since they are not stable for a trip to radiology for confirmatory CT or V/Q study, and physicians can be faced with the difficult decision to give thrombolytics or consult CT surgery/IR with minimal studies.
- As a risk stratification tool after dx of PE is made on CT or VQ scan, bedside echo with signs of acute RV strain should prompt admission to a higher level of care for monitoring (step-down or ICU) and consideration of additional therapies (catheter-based lyrics, surgical thrombectomy or IV tPA).
Signs of Right Ventricular strain on bedside echo include:
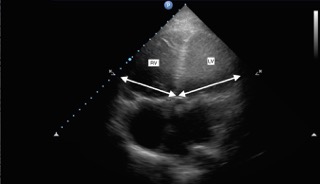
- Enlarged RV as evidenced by RV: LV ratio of 1:1 or greater. Basically, look to see if RV diameter is equal to or larger than the LV. This is best visualized in the apical-4 cardiac window.
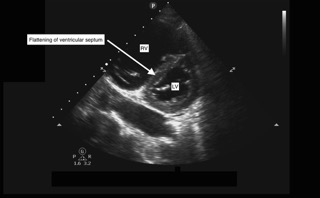
Septal D sign: As the right-sided pressures in the heart increase due to a large clot burden in the pulmonary arteries, this pushes the inter-ventricular septum from the right to the left, resulting in a flattening of the septum. The LV will appear like a capital “D” instead of a capital “O”. The parasternal short axis cardiac window is the best view to visualize this sign.
- McConnell’s Sign: sparing of cardiac motion at the RV apex with hypokinesis of the rest of the RV free wall. Also know as “apical wink” – this sign is though to be specific for acute RV strain.
- RV wall thickness: Patients with cor pulmonale or pulmonary HTN will have chronic RV dilatation. The RV myocardium compensates for higher pressures with hypertrophy of the muscle wall over time. An acute large PE occurs too quickly for RVH to develop, so the RV wall will not be thick. If you’re able to measure the RV free wall, and it is 4 mm or less, that is suggestive of acute process.

