A thin, 25-year-old male presented to the emergency department with 24 hours of moderate, colicky abdominal pain that eventually localized to his right lower quadrant. The pain was associated with anorexia, fever, nausea, and one episode of vomiting. A PGY-2 Resident scanning under the supervision of an Attending performed a bedside ultrasound to evaluate for possible appendicitis. They diligently recorded their positive scan, which they used to expedite his transfer to the OR.
Later, our PGY-3 Resident saw a patient who similarly presented with abdominal pain that localized to the RLQ within a few hours. He performed a bedside ultrasound to evaluate for appendicitis.
He was able to find the appendix quite easily.
See?
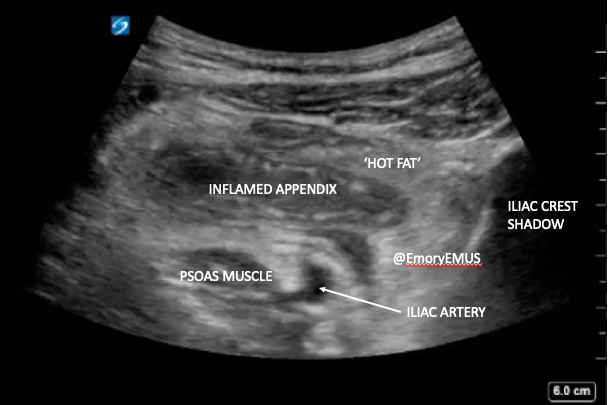
There is also some ‘hot fat’ surrounding the inflamed appendix. This is increased echogenicity of edematous fat that is analogous to fat stranding on CT.
You can have your patient localize the point of maximal tenderness for you and start scanning there. However, if you don't find the appendix easily:
- Have the patient cross their right leg over their left. This can help bring the appendix forward.
- Landmarks can help: scan around until you find the iliac crest laterally (hyperechoic cortex adjacent 'clean' shadow).
- Then move your probe toward the umbilicus (medially) until you find the iliac artery (most medial) and psoas muscle.
- Slide up and down the iliac artery until you see the appendix overlying it.
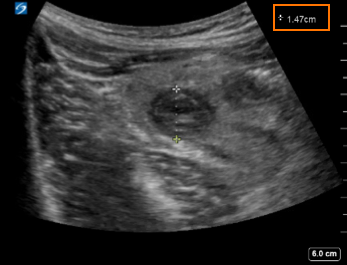
- Don’t forget to turn your probe and measure it in both transverse and sagittal planes.
In children and adults with a normal BMI, the linear (vascular) probe is often sufficient, because the appendix is usually visible under the depth of 6cm. Otherwise, you may need to use the curvilinear (abdominal) probe.
You may recall that the location of the appendix can be highly variable. Our PGY-3 Resident was confident this was the appendix because he found relevant landmarks:
- The iliac crest (lateral to the appendix)
- The iliac artery (medial to the appendix)
- Psoas muscle (deep to the appendix)
He increased his confidence that the structure was an inflamed appendix by confirming the structure was:
- "blind-ending"
- tubular
- outer to outer wall diameter >6mm
- non-compressible (unless there is sizable perforation)
- aperistaltic
You will earn bonus points if you see...
-
- Appendicolith/fecalith within the lumen (hyperechoic with posterior shadowing)
- Free fluid surrounding the appendix
- A "ring of fire" -- increased vascularity around the appendix using color-flow Doppler
Ultrasound is much more specific than sensitive for appendicitis. In a 2017 single-center study, doctors of all training levels were able to diagnosis appendicitis in patients using POCUS with a specificity of 98% and a sensitivity between 40 and 80% (depending on experience). This was after minimal training.
The physicians on these cases are all smart and capable … just like you. You can look at a grid of red and black lines and decide if a patient is having a heart attack. You can put wires down people’s necks down towards their hearts for life-sustaining medications. You can find the appendix with ultrasound. We believe in you.
Author: Tricia A. Smith, MD, MPH
2021

